Hip replacement is needed when a hip is affected by osteoarthritis, a condition where the hip joint becomes painful and stiff due to general wear and tear over the years. It is also done when the hip is affected by other types of arthritis such as rheumatoid arthritis.

The primary aim of hip replacement is to reduce pain. The pain you may be experiencing may be in the groin and also in the knee region on the same side. This is due to the hip and knee sharing a common nerve. In addition you may also be suffering from significant stiffness in the joint thus making day to day activities rather difficult. You may be experiencing pain at night. Often you will find the mornings are particularly difficult and the pain somewhat improves as the day progresses.
Not all hips with osteoarthritis need replacement. You will be tried on pain killers and anti-inflammatory medication in the first instance. You will also do some physiotherapy to improve the muscles around the hip joint and may also be tried with a walking aid.
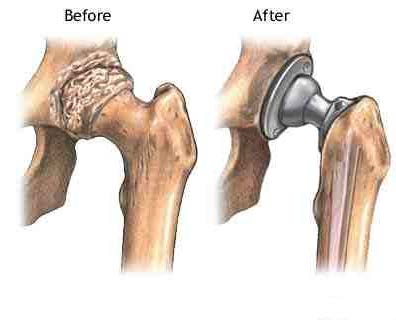
Hip replacement should improve your pain immensely. The improvement in mobility is secondary to the improvement of underlying pain. However, you must be aware that no artificial joint will be as good as your previously healthy natural joint. Nonetheless, hip replacement is generally a very successful operation.