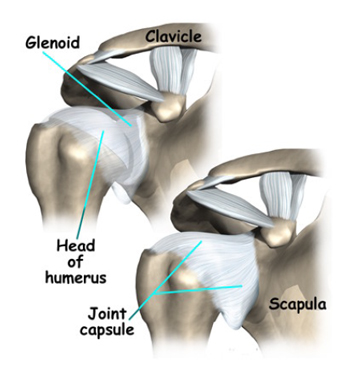
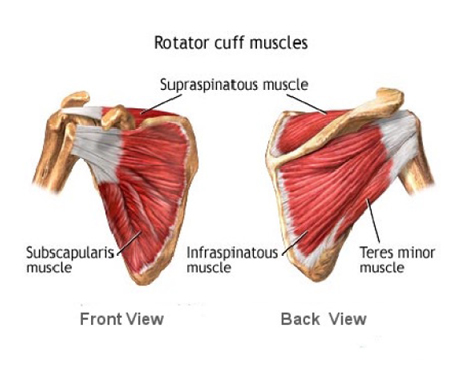
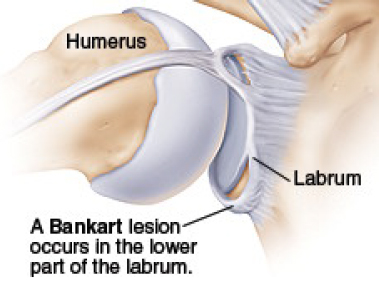
The benefit of the huge range of movements at the shoulder is that we are able to position the hand as required, the cost is that the shoulder is more likely to dislocate than any other joint. Unlike the hip which is a true ball and socket joint, the gleno-humeral joint of the shoulder is more like a ball on a saucer held in position by various soft tissues such as the labrum (the rubbery edge of the socket), the capsule and the ligaments which take the form of thickened areas within the joint capsule. The rotator cuff muscles are also crucial in maintaining stability.
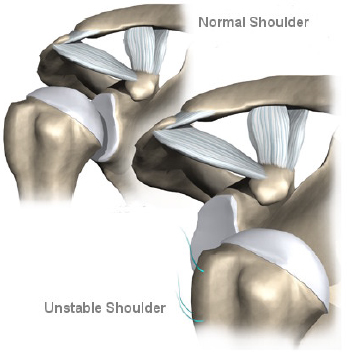
The term dislocation implies that the ball (humeral head) displaces completely from the glenoid (socket) whereas subluxation implies that the degree of displacement is less than dislocation in other words the humeral head retains some contact with the glenoid.
For those individuals who have loose or stretchy ligaments (sometimes termed double jointed) subluxation or even dislocation may be a regular and normal occurrence which causes no problems.
On the other hand if a traumatic dislocation occurs as a result of a fall or on the sports field subsequent episodes of instability whether subluxation or dislocation may be extremely distressing and painful. Some of you may have required relocation (reduction) of the shoulder in hospital under sedation or anaesthesia. In the young sports person after a first dislocation the likelihood of further dislocations is around 50%.
In patients over the age of 50 the risk of recurring dislocation is less, however there is a much higher chance of damage to the rotator cuff tendons. For those individuals with ligamentous laxity (sometimes termed multidirectional instability) a relatively minor injury may render an apparently normal shoulder painful and disabling. So in summary troublesome (symptomatic) instability may be due to ligamentous laxity, injury or a combination of the two.
The diagnosis is usually achieved on the basis of history and examination.
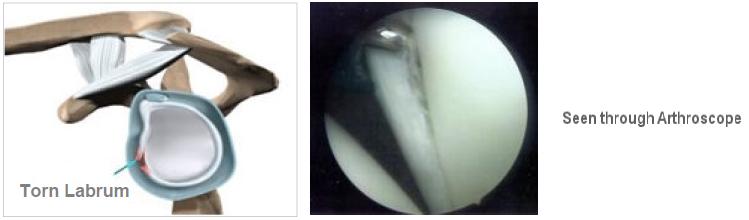
Additional information may be available from specialised imaging such as contrast CT or MRI which involves scanning after an injection into the shoulder joint which provides fine detail of the injured structures. In the event of an anterior dislocation (forward displacement of the humeral head) a scan may confirm damage to the structures on the front of the glenoid namely labrum, capsule, ligament and possibly the bony edge of the socket.
In the situation of multidirectional instability it may be difficult to identify any abnormality on the scan. This information is useful to the surgeon in deciding what type of operation if any is appropriate.
Sometimes physiotherapy is of help in controlling multidirectional instability. However recurrent anterior dislocation generally requires surgical stabilisation. Surgical techniques used vary from patient to patient and also between surgeons. However the rehabilitation and recovery periods are much the same. As a rule you can expect about six months to pass from surgery before the shoulder is comfortable and functional.
Traditionally surgery was carried out by open technique that is through an incision on the front of the shoulder dissecting between and preserving the superficial muscles. In the last ten years arthroscopic (keyhole) techniques have gained popularity and for the right patient in the hands of an appropriately trained surgeon the results are much the same, the only real difference in the long term is the size of the scar.
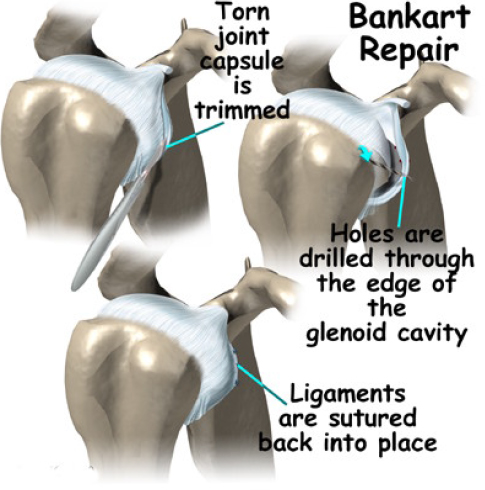
If the history is of traumatic dislocation then the primary aim will be reattachment of the torn labrum ligaments and capsule to the front of the glenoid using suture anchors.
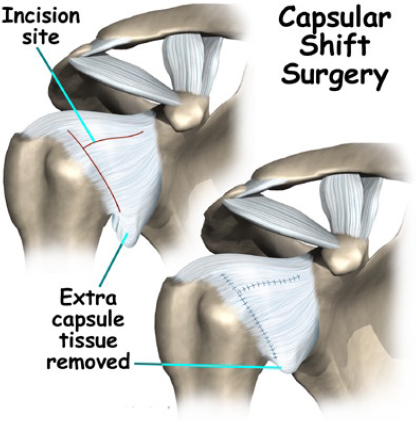
For multidirectional instability, capsular shift (tightening of the capsule) may be necessary to reduce subluxation.
With a prolonged history of recurrent dislocation a combination of reattachment and capsular shift procedures is performed. Occasionally when recurrent dislocation has caused significant bony damage to the front of the glenoid or in high demand individuals such as those who play regular sport an open procedure is necessary to screw a block of bone graft onto the front of the glenoid. The graft is usually harvested from the coracoid, a neighbouring part of the shoulder blade. Assuming the right procedure is done by a competent surgeon the likelihood of success with stabilisation is over 90% although it is important to emphasise that in those with lax ligaments (multidirectional instability) instability can recur as the tissues stretch over several years.
The procedure generally involves one overnight stay although after arthroscopic surgery it may be possible to go home the same day. Prior to admission you should have attended the pre-assessment clinic for assessment of your general health.
If you are coming into hospital on the day of your surgery it is important that you do not eat for six hours or drink for two hours prior to your admission to hospital. (Only drink black tea, black coffee or water). Bring loose comfortable clothing into hospital without awkward or numerous fastenings
On admission you will be examined by an anaesthetist who will assess your fitness for surgery and discuss the type of anaesthetic including regional block which may render your arm numb for about 12 hours after surgery. A pre-medication drug may be prescribed before your operation to help you relax. You will be asked to wear a theatre cap and gown and a nurse and porter will escort you to theatre.
On return to the ward you may expect:
- An oxygen mask on your face, this is removed on the anaesthetist’s instructions
- Temporary numbness and weakness of the arm if you have had a regional block
- A degree of pain. There will be pain relief prescribed, please ask the nurse if you require it so that you can be kept as comfortable as possible.
- A large bulky dressing on your shoulder for support
- A broad arm sling or anti-rotation sling, depending on the procedure carried out
On discharge an appointment will be provided with your surgeon usually three weeks following surgery. If you have any problems with your wound you should contact the hospital to have this checked.
Check X-ray of the shoulder is occasionally required. You will be fitted with a shoulder immobiliser sling before discharge, unless otherwise specified by your surgeon this is worn for three weeks after the operation although you are at liberty to loosen the sling and take the arm out for hygiene and washing purposes. Five days from operation the dressings can be removed and the sutures trimmed if absorbable or removed if non-absorbable, this is usually best done at the general practitioner’s surgery. At the three week stage the sling is discarded, physiotherapy is at the discretion of the surgeon, in general the aim is to slowly regain close to normal range of movement by three months from the operation. If necessary more forcible exercises can be initiated at three months along with muscle strengthening which can be done at home, in the gym and in the swimming pool. Contact sports and heavy overhead tasks must be avoided for six months from operation unless otherwise instructed.